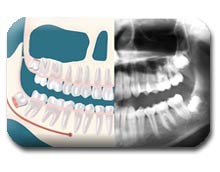
What are wisdom teeth?
Wisdom teeth, officially referred to as third molars, are usually the last teeth to develop. They are upper and lower teeth whose function is to grind food as part of the digestive process. They are located in the very back of your mouth, next to your second (or twelve year) molars and near the entrance to your throat. They usually complete development between the ages of 15 and 20, a time traditionally associated with the onset of maturity and the attainment of Wisdom.
Why should I have my wisdom teeth removed?
Since the wisdom teeth are the last to develop, they will not have enough room to adequately erupt into the mouth to become fully functional and cleansable teeth. This lack of room or space can result in a number of harmful effects on your overall dental health.
When this occurs they are said to be impacted, indicating their inability to erupt into an alignment which will allow them to be able to function in the chewing process. There are several types of impactions:
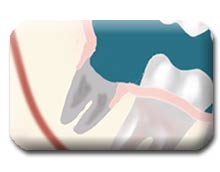
- Soft Tissue Impactions: There is adequate jaw bone to allow the wisdom tooth to erupt but NOT enough room to allow the gum tissue to recede to allow adequate cleaning of the tooth.
- Partial Bony Impactions: There is enough space to allow the Wisdom tooth to Partially erupt. It cannot function in the chewing process and creates cleaning problems, among others.

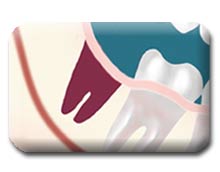
Complete Bony Impactions: There is NO space for the tooth to erupt. It remains totally below the jawbone or if even partially visible requires complex removal techniques.
Unusually Difficult Complete Bony Impactions: The impacted Wisdom tooth is in an unusual and difficult to remove position. This situation can also arise when the shape of the jawbone and other facial structures make removal of this tooth significantly more difficult.
If you do not have enough room in your mouth for your third molars to erupt and they become impacted, several detrimental results can occur:

Infection: Without enough room for total eruption, the gum tissue around the wisdom tooth can become irritated and infected, resulting in recurrent pain, swelling, and problems with chewing and swallowing.

Damage: If there is inadequate room to clean around the wisdom tooth, the tooth directly in front, the Second Molar, can be adversely affected resulting in gum disease (bone loss) or cavities (more appropriately known as dental caries or decay).

Disease: Non-infectious diseases can also arise in association with an impacted wisdom tooth. Cysts are fluid-filled ‘balloons’ inside the jawbone which are associated with impacted wisdom teeth and slowly expand destroying adjacent jawbone and occasionally teeth. They can be very difficult to treat if your wisdom teeth are not removed in your teenage years. Although rare, tumors can be associated with the delayed removal of wisdom teeth.

Crowding: Although controversial, many feel that impacted wisdom teeth directly contribute to crowding of your teeth which is most noticeable in the front teeth, usually the lower front teeth. This is most commonly seen after a patient has had braces. There are most likely a number of factors that cause teeth to crowd after braces or in early adulthood and retained, impacted wisdom teeth are likely to play a contributory role. Although wisdom tooth removal cannot be recommended solely to avoid crowding, it can be recommended to absolutely eliminate its possible role in future crowding and other bite changes.
Unless you have an active problem at the time of your consultation, the reason for removal is primarily preventative to avoid long term problems.
We will need to see you for a consultation before it is determined IF you will benefit from Wisdom tooth removal. We will need to take a special x-ray of your mouth and jaws to determine how much room you have, if any, for your Wisdom teeth to erupt.
So, do I really have to have them all removed?
In most cases the absolute answer is no. Unless you have been told that you have a life-altering disease process (which is unlikely), you don’t have to do anything until or unless YOU chose to do so. This is not critical, life-saving, emergent medical treatment. It is elective. We understand, however, that we can identify problematic patients early in their teens and treat them when the impact of the surgery is minimal and their ability to recover is at its maximum.
What is the best age to have wisdom teeth removed?
If it is recognized that you do not have enough room in your mouth for your third molars to erupt, it is advisable to have them removed as soon as it is recognized. In some patients it is as early as 11 or 12 whereas in others it may not be until 17 or 18 years of age. You will heal faster, with more predictable final healing, and have fewer complications than an older patient.
What if I don’t have my wisdom teeth removed now?
Many people, especially in years past, were told to take a “wait and see” approach to wisdom teeth. Many who did not have adequate room developed localized problems previously mentioned. The problem with this approach is that IF it is necessary to remove impacted wisdom teeth in your thirties, forties, fifties, or beyond, it is clearly more difficult for you as the patient. The post-operative course is usually prolonged and there is a higher complication rate. Treating these complications is more difficult than with a younger patient. IF you do not have your impacted wisdom teeth removed in your teenage years or early in your twenties, it may be advisable to wait until or unless a localized problem (such as cyst formation or localized gum disease and bone loss) develops and then treat the affected area only. This is because the predictability of healing decreases with age and the likelihood of infection and delayed healing increases.
If I decide to do it, when should I have them removed?
First of all, you need to decide if you will be sedated (‘go to sleep’). Most people clearly prefer to be unaware of the experience when they have their Wisdom teeth removed. You will be provided with appropriate anesthesia options for you at your consultation.
All outpatient surgery is performed under appropriate anesthesia to maximize your comfort. Our office staff has the training, license, and experience to provide various types of anesthesia to allow patients to select the most appropriate alternative. These services are provided in an environmental of optimum safety, utilizing modern monitoring equipment and staff experienced in anesthesia techniques. The Surgical Care Team, the office facilities and myself are inspected on behalf of the New Hampshire Board of Dental Examiners on a regular basis.

On the day of your procedure, you will take medications to help minimize post-operative pain and swelling. We ask that a parent or responsible adult accompanies you to the office and plans to stay with you the rest of the day. Your procedure will take about an hour and you will probably be in the office for 1-2 hours. Recent advances in medicine and technology allow patients to undergo wisdom tooth removal in a manner, which promotes rapid healing and minimal post-operative discomfort. State of the art sterilization and infection control techniques are used at all times, including the use of sterile water for irrigation during surgery. The evening before your surgery , I would like you to take an anti-inflammatory medication, frequently 800 mg of ibuprofen (also called Motrin and the same as 4 Advil), which I prescribed, before you go to bed (unless otherwise instructed). This medication prevents pain and swelling.

On the morning of your surgery, you should not have anything to eat or drink except for what I have provided for you in the form of prescription medication. I would like you to take antibiotics with small sips of water approximately one hour prior to the surgery. Usually, this antibiotic is amoxicillin. Occasionally, the antibiotic will be changed if you have an allergy to amoxicillin or penicillin or if you have taken similar antibiotics immediately before your appointment. I would also like you to take one ibuprofen 800 mg pill with some water as well one hour prior to surgery. These will be taken on an empty stomach, and it usually does not cause stomach upset prior to the surgery. Remember also to bring somebody with you so that they can drive you home after the surgery is performed.
When you are seated in the Surgical Room, you will be placed on nitrous oxide, which will make you more comfortable. After this, we will start an IV in your arm. This will be done using freezing spray that will make your skin quite cold so you won’t feel the actual IV being placed. The medication will be administered through a vein in your arm. Remember, that with the intravenous sedation techniques used in this office, you may be vaguely aware of the surgical procedure being performed. You will be relaxed, quite sleepy, and with the use of local anesthesia you should feel minimal, if any, discomfort during the procedure. We have found that most patients are not aware of the procedure being performed . When you wake up from the anesthesia, you will be comfortable. We will have given you local anesthesia so you won’t be in any pain, and you will still be somewhat sleepy.
Our surgical assistants will review your post-operative instructions. When you leave the office you will be comfortable and drowsy. Most patients prefer to go home and rest with no other physical or scholastic activities planned for a few days. DO NOT WORRY ABOUT STITCHES . Stitches (also known as sutures) are usually placed to control bleeding, aid healing and help prevent food from collecting in the surgical site – – especially for lower teeth. The sutures we use dissolve in 3 to 5 days and DO NOT HAVE TO BE REMOVED.
When you arrive home, the local anesthesia will start to wear off and then you may have some discomfort. Please remember to take another ibuprofen 800 mg as the local anesthesia is wearing off. If the ibuprofen is enough to control your pain, stay on the ibuprofen every six to eight hours as needed. If you find the ibuprofen is not adequate for pain, I also prescribe a stronger pain medication. This stronger medication is usually Percocet (also known as Roxicet or oxycodone with acetaminophen). I would much prefer that you take only one-half tablet of Percocet only if the ibuprofen (Motrin) is not working adequately, and only if you have been able to get some type of food in your stomach. The reason for this is that the Percocet can cause you a lot of stomach upset, nausea, and vomiting. I would recommend that you try to get some clear carbonated beverages, such as ginger ale, Seven-Up, or Sprite, in your stomach prior to even taking any of the Percocet. Whatever you do, please do not start out with the Percocet or take a whole pill of Percocet as this can lead to nausea and vomiting.
After you arrive home and six hours following the surgery, you should take another dose of the antibiotic you were given. This one-day course of antibiotics usually will control infection. Ninety-five percent of the time, if you take one day’s worth of an antibiotic, you will not get an infection. Realize, of course, that 5% of the time, you will still get an infection and will be required to take antibiotics for one week. If this happens, please don’t hesitate to call the office. You may recognize signs of this occurring if you notice more swelling, more pain, more redness, and it doesn’t seem to be improving on the third or fourth day. Please call us if you have any questions.
If you are given antibiotics and you take birth control pills, you should be aware that the birth control pill might become ineffective and take appropriate precautions.
What happens afterwards…what will I feel like?
On the first day after surgery, you do experience some bleeding and some pain. You should cover your pillowcase with something so that you don’t get any blood on it. Each individual’s reaction to surgery varies, and the sensation of pain can range from mild discomfort to severe pain. You can expect approximately two to four days of discomfort before noting improvement. The second day, you will still have some swelling.
A variable amount of swelling can be expected following the surgery. This swelling usually peaks on the second day and should begin resolving on the third day. You can limit the amount of swelling you will have by using ice for the entire first day. The more ice you have on the first day, the less swelling you will have on the second day. Please remember to put ice on the first day even if it’s somewhat uncomfortable to have the cold next to your skin. Wear the Ice Wrap we provide.
On the third day, you will notice that your jaw muscles are stiff, and it’s difficult to open your jaw as wide as you used to. This will resolve with the help of moist heat. Actually, moist heat is preferred after the first day. You can apply moist heat to your face on the second and third day, and this will allow your muscles to relax more and open wider.
Most of the time you will want to maintain a low profile for a few days. We ask that you follow your post-operative instructions closely as they will make you most comfortable during the first few days following your procedure. Please allow the time to let your body begin healing before resuming an active social, academic, or athletic schedule. Most patients feel like they are over the hump in 3-5 days.
Are there any problems?
As with any medical procedure, there can be complications or an unanticipated result that you should be aware of:
There is a nerve, which supplies feeling to the lower lip, chin, and tongue which is frequently very close to the roots of the lower wisdom teeth. Having these teeth out between the ages of 12 and 18 usually provides shorter roots so that the nerve is not so close to the roots of these teeth. Occasionally, when the teeth are removed, especially in older patients, the roots have grown longer and become closer to the nerve itself. This nerve can become irritated in the process of removing the tooth. When local anesthesia wears off, you may experience a tingling or numb sensation in the lower lip, chin, or tongue. Should this occur, it is usually temporary and will resolve gradually over a period of weeks or months. RARELY, it can result in a permanent alteration of sensation similar to the feeling of Novocain. We feel that you should be aware of this before consenting to surgery.

The upper wisdom teeth are situated close to your sinuses, and their removal can result in a communication between your mouth and the sinus. Once again, if the teeth are removed at an early age, the root formation is minimal, and this complication is very unlikely to occur. Should this occur, it will usually close spontaneously. We may give you special instructions to follow if this is apparent at the time of surgery. I prefer that you don’t blow your nose for two or three days following the surgery. You can wipe your nose, but don’t blow your nose. If you have to sneeze, you should sneeze with an open mouth into a tissue – – you should not create any pressure in the sinus area, which may dislodge the healing blood clot. If you sense a communication occurring after the surgery, please contact the office. RARELY, an additional procedure may be necessary to close the communication.
Dry sockets continue to be the most common problem people experience following dental surgery. They arise due to premature loss of a blood clot in the empty tooth socket. This seems to occur with greater frequency in people who smoke or are taking birth control pills. While both jaws can be affected, they usually occur in the lower jaw on the third to fifth day. They cause a deep, dull, continuous aching on the affected side(s). Patients may first notice the pain starting in the ear radiating down towards the chin. It frequently begins in the middle of the night, and the Motrin medication usually doesn’t help.
Treatment involves placing a medicated dressing in the “empty” tooth socket. This will help decrease the pain and protect the socket from food particles. The effectiveness in alleviating the pain lasts for 24-48 hours and usually will require dressing changes every day or two for five to seven days. Dressings usually are removed when you have been pain free for 2-3 days. The dressing doesn’t aid in healing. The only reason to place a dressing is for pain control. If Motrin is controlling the pain, the socket will heal without a dressing. An irrigation device will be given to you to help keep food particles from lodging in the extraction site following removal of the dressing.
Occasionally, post-operative infections occur. This usually requires an office visit and clinical examination. Many times, just placing you on an antibiotic for one week will take care of the infection. It will occasionally require drainage of the infected area, which may have accumulated near the surgical site, and even more rarely do the patients need to be admitted to the hospital for intravenous antibiotics and further surgical drainage.
Other temporary problems you may experience in the postoperative period include stiffness of the jaws, chafing around the corners of your lips, facial bruising, and blood oozing from the extraction sites. The postoperative instruction sheet we will provide should answer many of the questions related to these more common concerns. If not, don’t hesitate to call the office.
What does it cost…and does insurance cover it?
Because of the different types of impacted wisdom teeth, along with different anesthesia options, it is impossible to give you a realistic estimate of what our services will cost until we have reviewed your x-rays.
Every insurance company has a different policy regarding the extent of coverage for a given surgical procedure. We encourage you to check with both your medical AND dental insurance carrier to determine your coverage and out of pocket liability.
What if I have questions before surgery?
If this information, combined with information you receive at your consultation appointment doesn’t answer all of your questions, please call the office to speak to one of our Patient Care Coordinators: 603-436-8222.

